- For US Healthcare Providers
- Full Prescribing Information
FOR ADULTS WITH ACTIVE PsA
DEMONSTRATED JOINT SYMPTOM CONTROL IN ACTIVE PsA
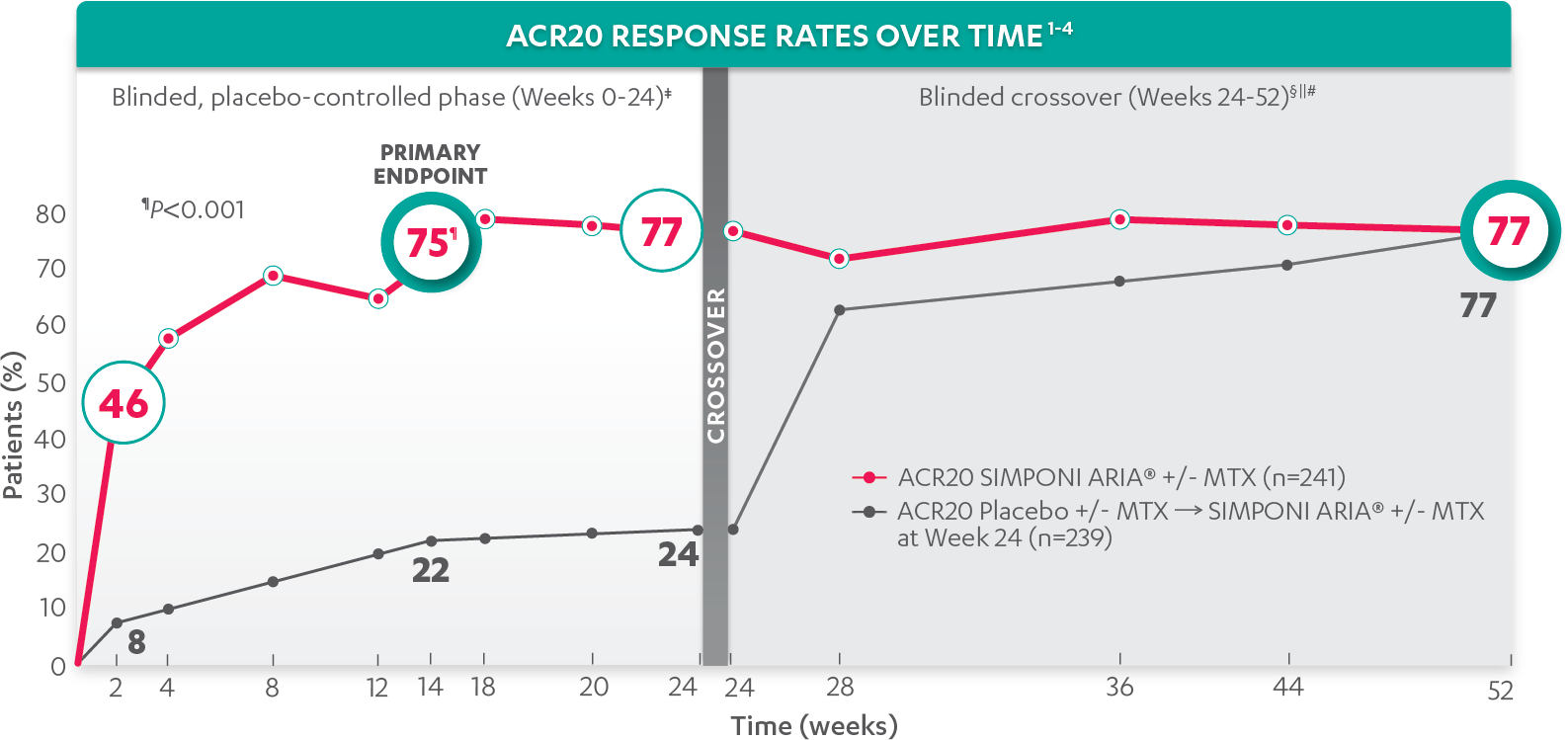
ACR20 response at Week 14 (primary endpoint) vs placebo*†‡:
75%
of patients receiving SIMPONI ARIA® +/- MTX (181/241) achieved ACR20 response (P<0.001)
VS
22%
of patients receiving placebo +/- MTX (52/239)1-3
ACR20 response in patients receiving SIMPONI ARIA® + MTX was similar to those receiving SIMPONI ARIA® without MTX
Rapid ACR20 response at Week 2*†‡:
46%
of patients receiving SIMPONI ARIA® +/- MTX (110/241) achieved ACR20 response
VS
8%
of patients receiving placebo +/- MTX (18/239)1-3
ACR20 responses at Week 2 were not adjusted for multiplicity. Therefore, statistical significance has not been established.
ACR20 RESPONSE AT WEEK 24*†‡:
77%
of patients receiving SIMPONI ARIA® +/- MTX (185/241) achieved ACR20 response
VS
24%
of patients receiving placebo +/- MTX (58/239)1-3
ACR20 responses at Week 2 and Week 24 were not adjusted for multiplicity. Therefore, statistical significance has not been established.
ACR20 response at Week 52§ǁ¶:
77%
of patients receiving SIMPONI ARIA® +/- MTX achieved ACR20 response
VS
77%
of patients receiving placebo +/- MTX who crossed over to SIMPONI ARIA® +/- MTX2,4
*The same patients may not have responded at each time point.
†ACR20 responses are based on imputed data using treatment failure, last observation carried forward (LOCF) for partially missing data, and nonresponder imputation (NRI) for completely missing data.
‡In this intention-to-treat (ITT) analysis, patients were considered to be nonresponders if they experienced any of the following: increased the dose of MTX or oral corticosteroids over baseline for PsA not as part of early escape; initiated treatment with DMARDs, systemic immunosuppressives, treatment with oral, intravenous (IV), or intramuscular (IM) corticosteroids, and/or biologics for PsA; met early escape criteria at Week 16 and started concomitant medication intervention; or discontinued treatment due to an unsatisfactory therapeutic effect.
§Treatment failure criteria were not applied after Week 24.
ǁAt Week 24, all remaining patients in the placebo +/- MTX group began receiving SIMPONI ARIA® +/- MTX in a blinded manner. At Week 24, subjects in the SIMPONI ARIA® +/- MTX group received a placebo infusion to maintain the treatment blind, and then continued to receive SIMPONI ARIA® +/- MTX at Week 28 and q8w thereafter through Week 52.
¶After Week 24, patients and doctors knew that all patients were on SIMPONI ARIA® (blinded active treatment), which may have affected the results.
Study design: GO-VIBRANT was a global, multicenter, randomized, double-blind, placebo-controlled study evaluating the efficacy and safety of SIMPONI ARIA® compared with placebo in 480 adult patients with active PsA. The target study population was biologic-naïve patients with active PsA for ≥6 months who met ClASsification criteria for Psoriatic ARthritis (CASPAR) criteria at screening. Patients in this trial had a diagnosis of PsA for at least 6 months and had symptoms of active disease (≥5 swollen joints and ≥5 tender joints and a CRP level of ≥0.6 mg/dL). At Week 0, patients were randomized in a 1:1 ratio to 1 of 2 treatment groups. Patients were allowed to be treated with or without MTX. Patients in the placebo group (n=239) were randomized to receive IV placebo infusions at Weeks 0, 4, 12, and 20. Patients in the SIMPONI ARIA® group (n=241) were randomized to receive SIMPONI ARIA® 2 mg/kg infusions at Weeks 0, 4, and q8w thereafter through Week 52. Patients were to receive a placebo infusion at Week 24 to maintain the treatment blind. At Week 24, all patients switched to treatment with SIMPONI ARIA® 2 mg/kg and were to receive administrations at Weeks 24, 28, and q8w through Week 52. The primary endpoint was the percentage of patients achieving an ACR20 response at Week 14.
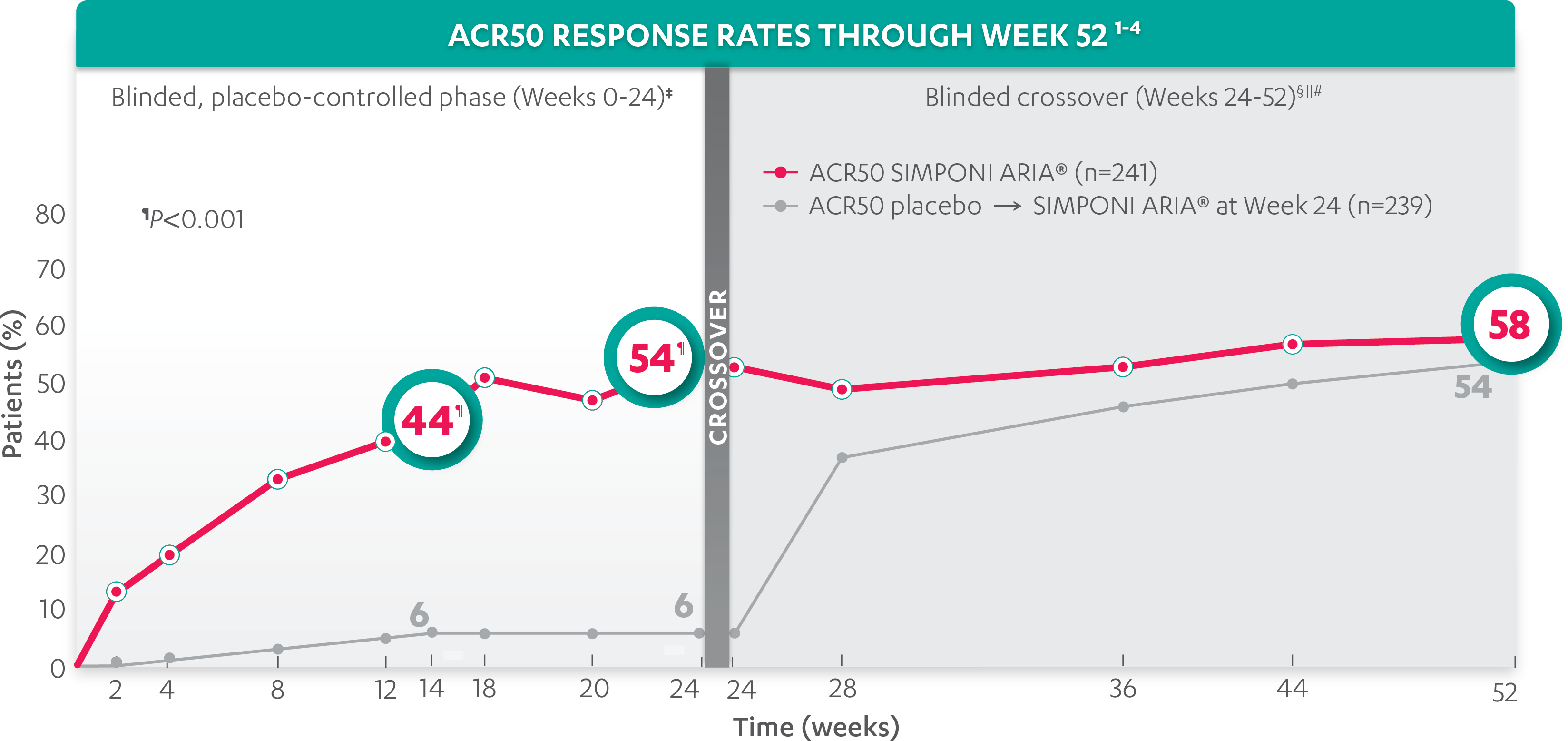
ACR50 response at Week 14 vs placebo*†‡:
44%
of patients receiving SIMPONI ARIA® +/- MTX (105/241) achieved ACR50 response (P<0.001)
VS
6%
of patients receiving placebo +/- MTX (15/239)1-3
ACR50 response at Week 2*†‡:
13%
of patients receiving SIMPONI ARIA® +/- MTX (31/241) achieved ACR50 response
VS
0.4%
of patients receiving placebo +/- MTX (1/239)1
ACR50 response at Week 24*†‡:
54%
of patients receiving SIMPONI ARIA® +/- MTX (130/241) achieved ACR50 response (P<0.001)
VS
6%
of patients receiving placebo +/- MTX (14/239)1-3
ACR50 responses at Week 2 were not adjusted for multiplicity. Therefore, statistical significance has not been established.
ACR50 response at Week 52§ǁ¶:
58%
of patients receiving SIMPONI ARIA® +/- MTX achieved ACR50 response
VS
54%
of patients receiving placebo +/- MTX who crossed over to SIMPONI ARIA® +/- MTX2,4
*The same patients may not have responded at each time point.
†ACR50 response is based on imputed data using treatment failure, last observation carried forward (LOCF) for partially missing data, and nonresponder imputation (NRI) for completely missing data.
‡In this intention-to-treat (ITT) analysis, patients were considered to be nonresponders if they experienced any of the following: increased the dose of MTX or oral corticosteroids over baseline for PsA not as part of early escape; initiated treatment with DMARDs, systemic immunosuppressives, treatment with oral, intravenous (IV), or intramuscular (IM) corticosteroids, and/or biologics for PsA; met early escape criteria at Week 16 and started concomitant medication intervention; or discontinued treatment due to an unsatisfactory therapeutic effect.
§Treatment failure criteria were not applied after Week 24.
ǁAt Week 24, all remaining patients in the placebo +/- group began receiving SIMPONI ARIA® +/- MTX in a blinded manner. At Week 24, subjects in the SIMPONI ARIA® +/- MTX group received a placebo infusion to maintain the treatment blind, and then continued to receive SIMPONI ARIA® +/- MTX at Week 28 and q8w thereafter through Week 52.
¶After Week 24, patients and doctors knew that all patients were on SIMPONI ARIA® (blinded active treatment), which may have affected the results.
Study design: GO-VIBRANT was a global, multicenter, randomized, double-blind, placebo-controlled study evaluating the efficacy and safety of SIMPONI ARIA® compared with placebo in 480 adult patients with active PsA. The target study population was biologic-naïve patients with active PsA for ≥6 months who met ClASsification criteria for Psoriatic ARthritis (CASPAR) criteria at screening. Patients in this trial had a diagnosis of PsA for at least 6 months and had symptoms of active disease (≥5 swollen joints and ≥5 tender joints and a CRP level of ≥0.6 mg/dL). At Week 0, patients were randomized in a 1:1 ratio to 1 of 2 treatment groups. Patients were allowed to be treated with or without MTX. Patients in the placebo group (n=239) were randomized to receive IV placebo infusions at Weeks 0, 4, 12, and 20. Patients in the SIMPONI ARIA® group (n=241) were randomized to receive SIMPONI ARIA® 2 mg/kg infusions at Weeks 0, 4, and q8w thereafter through Week 52. Patients were to receive a placebo infusion at Week 24 to maintain the treatment blind. At Week 24, all patients switched to treatment with SIMPONI ARIA® 2 mg/kg and were to receive administrations at Weeks 24, 28, and q8w through Week 52. The primary endpoint was the percentage of patients achieving an ACR20 response at Week 14.
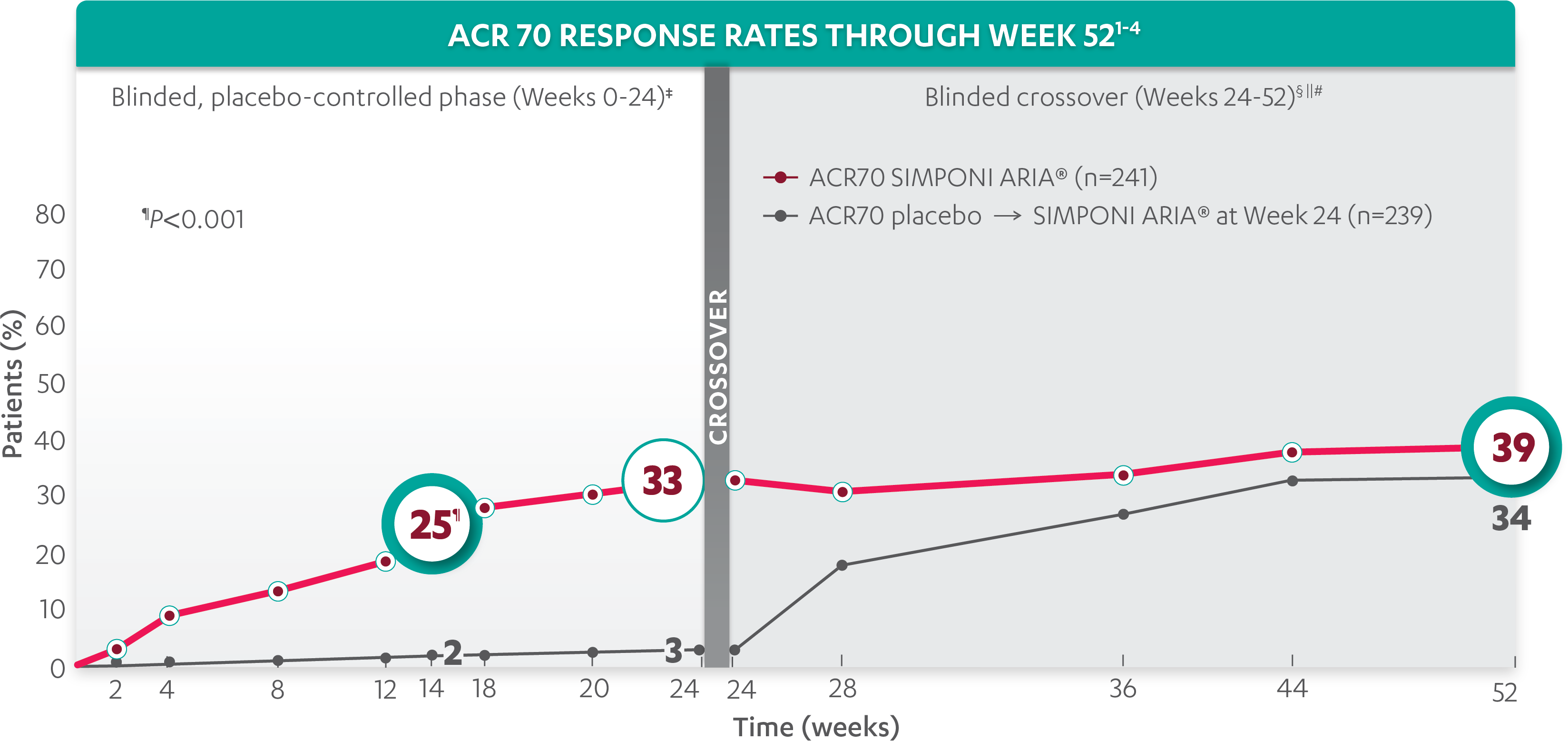
ACR70 response at Week 14 vs placebo*†‡:
25%
of patients receiving SIMPONI ARIA® +/- MTX (59/241) achieved ACR70 response (P<0.001)
VS
2%
of patients receiving placebo +/- MTX (5/239)1-3
ACR70 response at Week 24*†:
33%
of patients receiving SIMPONI ARIA® +/- MTX (79/241) achieved ACR70 response
VS
3%
of patients receiving placebo +/- MTX (8/239)1-3
ACR70 responses at Week 2 and Week 24 were not adjusted for multiplicity. Therefore, statistical significance has not been established.
ACR70 response at Week 52§ǁ¶:
39%
of patients receiving SIMPONI ARIA®+/- MTX achieved ACR70 response
VS
34%
of patients receiving placebo +/- MTX who crossed over to SIMPONI ARIA® +/- MTX2,4
*The same patients may not have responded at each time point.
†ACR70 response is based on imputed data using treatment failure, last observation carried forward (LOCF) for partially missing data, and nonresponder imputation (NRI) for completely missing data.
‡In this intention-to-treat (ITT) analysis, patients were considered to be nonresponders if they experienced any of the following: increased the dose of MTX or oral corticosteroids over baseline for PsA not as part of early escape; initiated treatment with DMARDs, systemic immunosuppressives, treatment with oral, intravenous (IV), or intramuscular (IM) corticosteroids, and/or biologics for PsA; met early escape criteria at Week 16 and started concomitant medication intervention; or discontinued treatment due to an unsatisfactory therapeutic effect.
§Treatment failure criteria were not applied after Week 24.
ǁAt Week 24, all remaining patients in the placebo +/- group began receiving SIMPONI ARIA® +/- MTX in a blinded manner. At Week 24, subjects in the SIMPONI ARIA® +/- MTX group received a placebo infusion to maintain the treatment blind, and then continued to receive SIMPONI ARIA® +/- MTX at Week 28 and q8w thereafter through Week 52.
¶After Week 24, patients and doctors knew that all patients were on SIMPONI ARIA® (blinded active treatment), which may have affected the results.
Study design: GO-VIBRANT was a global, multicenter, randomized, double-blind, placebo-controlled study evaluating the efficacy and safety of SIMPONI ARIA® compared with placebo in 480 adult patients with active PsA. The target study population was biologic-naïve patients with active PsA for ≥6 months who met ClASsification criteria for Psoriatic ARthritis (CASPAR) criteria at screening. Patients in this trial had a diagnosis of PsA for at least 6 months and had symptoms of active disease (≥5 swollen joints and ≥5 tender joints and a CRP level of ≥0.6 mg/dL). At Week 0, patients were randomized in a 1:1 ratio to 1 of 2 treatment groups. Patients were allowed to be treated with or without MTX. Patients in the placebo group (n=239) were randomized to receive IV placebo infusions at Weeks 0, 4, 12, and 20. Patients in the SIMPONI ARIA® group (n=241) were randomized to receive SIMPONI ARIA® 2 mg/kg infusions at Weeks 0, 4, and q8w thereafter through Week 52. Patients were to receive a placebo infusion at Week 24 to maintain the treatment blind. At Week 24, all patients switched to treatment with SIMPONI ARIA® 2 mg/kg and were to receive administrations at Weeks 24, 28, and q8w through Week 52. The primary endpoint was the percentage of patients achieving an ACR20 response at Week 14.